Clitorodynia
Clitoral Pain
Clitorodynia is a type of vulvodynia in which the pain localized to the clitoris. Once again, the suffix -”dynia” for pain, and “clitoro” to designate the location of the clitoris.
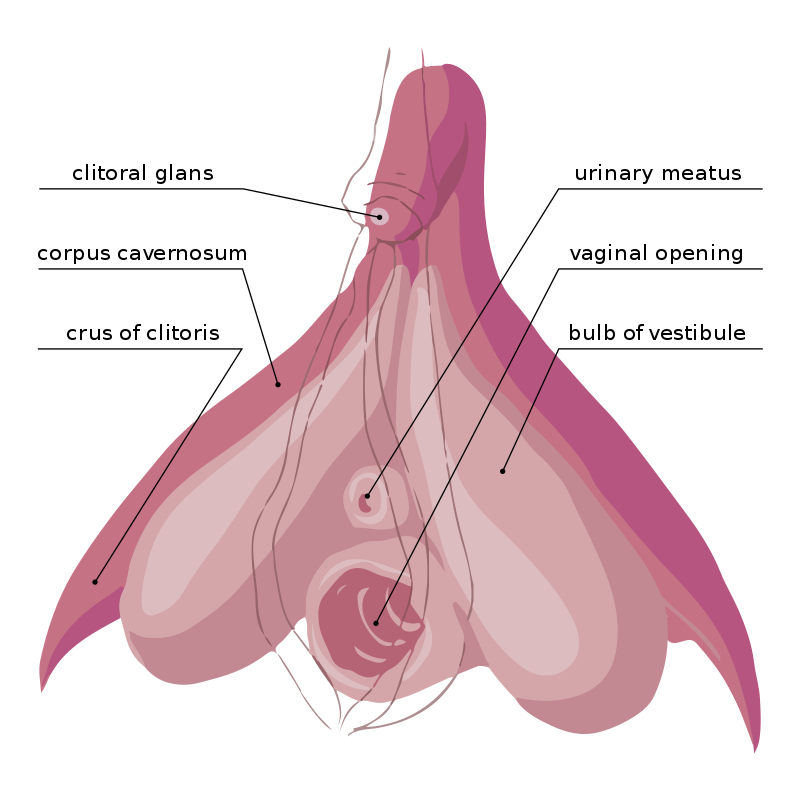
You might be surprised to learn how large your clitoris actually is! The clitoris is the homologous organ to the male penis, and is also a large, erectile organ. Also similar to a penis, the end is protected by a hood that is meant to be mobile. When the gland fills with blood, expands, and becomes erect, the hood should retract.
https://commons.wikimedia.org/wiki/File:Clitoris_Anatomy.svg
Clitoral Adhesions & Phimosis
The inability to retract the foreskin, called phimosis, is well understood in men. Urologists are familiar with this issue and how to treat it. A similar phenomenon occurs in women, referred to as clitoral adhesions or phimosis. The hood of the clitoris can become inflamed and even stuck (adhered) to the end of the clitoris, making the hood immobile. This can cause pain when the clitoris swells, but the hood is stuck down. Also, normal skin secretions can become trapped under the adhesions. Smegma is the fancy name for the oil secretions of the skin. (I’m pretty sure the word “smegma” is one of the only things I remember from my sub-par sex education classes in school.) Smegma trapped in an adhesion can cause more pain, especially if it causes inflammation/irritation or forms keratin pearls. Sexual medicine specialists that are also urologists are the perfect doctors to study clitoral adhesions!
New research is showing that clitoral adhesions might actually be very common in women with sexual dysfunction, more than 1 in 5. (1) However, only 20% of those women actually came in because of clitoral pain. (1) This is probably because a lot of women just accept their pain as “normal.” Also, most gynecologists are not trained to examine the clitoris, so if you assumed that your gynecologist would tell you if there was a problem, it might have been missed. This new study was published in an open access journal, meaning everyone can read the full article. I encourage you to go and see the photographs of a unaffected clitoris and various degrees of clitoral adhesions. (1) Do not be afraid to do a self exam and compare!
Clitoral adhesions can be lysed in the office. (1-2) Local anesthetics are using during the procedure and afterward for pain. A high success rate is reported for reduction in clitoral pain after the lysis procedure (86%). (2)
After the procedure, the women were told to soak in the tub and retract the hood daily to clean underneath. (2) And after healing too! Cleaning under the hood regularly is not just for penises, the same applies to the clitoris. I wish someone had told me that (especially since it is consistently taught to young boys).
Modified from: Miguelferig [CC0], from Wikimedia Commons https://commons.wikimedia.org/wiki/File:Vulva_hymen_miguelferig.png
Other causes of clitoral pain
Women also experience clitorodynia that is likely not caused by clitoral adhesions. Unfortunately, research is even more limited here. There was one recent study that collected data from women about their clitoral pain to look for patterns. (3) The results showed that pain can be either provoked or unprovoked, and is usually associated with other vulvar pain, but not always. (3) Clitoral pain can be caused by muscle dysfunction of the surrounding muscles, specifically the bulbocavernosus and ischiocavernosus. (4) Alternatively, a problem with central or local nerves could cause clitoral pain. A physical therapist may be well suited to help map the pain and determine if it aligns with a certain nerve or nerve branch. To see a diagram of the various nerves responsible for sensation and muscle control in the pelvic region, check out The Pelvic Guru’s resources. It is clear that there are many biologically distinct conditions and further research is needed to learn more.
I have moderate clitoral adhesions. I was diagnosed with them at the same time as my vestibulodynia diagnosis in December 2017. I decided not to deal with them at first and started with my other vestibulodynia treatments. Later on I considered doing the adhesion lysis in the office, in hopes of having something that didn’t hurt, but I ended up scheduling my vestibulectomy and decided to have the adhesions lysed during my surgery. After my surgery, unfortunately, the adhesions came back. I’m now using a topical steroid / anti-fungal to try to reduce the inflammation and thin the tissue (the clitoral hood was swollen/thickened).
References
1. Aerts L, Rubin RS, Randazzo M, Goldstein SW, and I Goldstein. 2018. Retrospective Study of the Prevalence and Risk Factors of Clitoral Adhesions: Women’s Health Providers Should Routinely Examine the Glans Clitoris. Sexual Medicine 6(2) 115-122. https://www.ncbi.nlm.nih.gov/pubmed/29559206 Open Access Direct Link: https://www.smoa.jsexmed.org/article/S2050-1161(18)30025-4/fulltext
2. Rubin R, Minton J, Gagnon C, Winter A, and I Goldstein. 2017. PD25-2 Taking Responsibility for Female Prepucial Disorders: Urologic Management of Phimosis-Based Clitorodynia. The Journal of Urology 197(4) Supplement e502. https://www.jurology.com/article/S0022-5347(17)31421-0/fulltext
3. Parada M, D’Amours T, Amsel R, Pink L, Gordon A, and YM Binik. 2015. Clitorodynia: A Descriptive Study of Clitoral Pain. The Journal of Sexual Medicine 12(8) 1772-80. https://www.ncbi.nlm.nih.gov/pubmed/26104318
4. Shafik A. 2000. The role of the levator ani muscle in evacuation, sexual performance and pelvic floor disorders. International Urogynecology Journal and Pelvic Floor Dysfunction 11(6) 361-376. https://www.ncbi.nlm.nih.gov/pubmed/11147745

![Modified from: Miguelferig [CC0], from Wikimedia Commons https://commons.wikimedia.org/wiki/File:Vulva_hymen_miguelferig.png](https://images.squarespace-cdn.com/content/v1/5c28ff4d297114a6e7ac1199/1553648242636-ZCDUOF6EJLK3085BDW71/Clitorodynia.jpg)